Over the past decade, Russia has seen a rising trend in cases of acute food poisoning. According to the World Health Organization, 2% of the population seeks medical attention annually due to mushroom poisoning.
Despite years of experience in diagnosing and treating this condition, initial diagnosis is complex and requires differentiation. Difficulties are often associated with the variety of toxicological symptoms and syndromes that arise from exposure to toxins. Due to the prevalence of acute mushroom poisoning, everyone should be aware of emergency treatment options.
How long does it take for the first symptoms to appear?
The time period when symptoms appear depends on many factors:
- type of poisonous mushroom;
- amount eaten;
- individual protective forces of the body and the functioning of the immune-humoral system.
The most highly toxic mushrooms are those of the genera Amanita (A.phalloides, A.virosa, A.verna, A.ocreata), Galerina (G.autumnalis, G.marginata), and Lepiota. The onset of symptoms averages six hours after ingestion.
For the amanita group, intoxication typically occurs within 24-48 hours. This has an adverse effect on patients, as all the toxins produced have already entered the bloodstream by this time, making treatment difficult.
The main symptoms of poisoning by plants and mushrooms
Depending on the type of mushroom consumed, the presence of certain toxins in them, the time that has passed from the consumption of the mushrooms to the first clinical manifestations, and the manifestation of typical symptoms and signs, a syndromic classification of mushroom poisoning is generally accepted.
Depending on the type of lesion
There are 3 groups of poisonings by poisonous mushrooms and plants:
- With gastroenterotropic action.
- With neurotropic action.
- With hepatonephrotropic action.

Group I poisoning is caused by eating different types of mushrooms (poisonous rowan, false sulfur-yellow honey fungus, false brick-red honey fungus, poisonous geranium, dark-striped geranium, poisonous entoloma, poisonous gray entoloma), which have in common the presence of irritating substances and biogenic amines in the mushrooms, which, as a rule, do not have a resorptive effect.
The clinical picture of poisoning is quite characteristic: rapid onset of illness (within 20 minutes, rarely within 2-3 hours of consumption), followed by gastroenteritis, which typically lasts from several hours to a day. In the absence of concomitant decompensated diseases, patients do not die. The prognosis is favorable.
Poisoning with poisonous plants and mushrooms of Group II most often results from the consumption of the rather dangerous Inocybe patujara (Amanita muscaria, Amanita panterina, Clitocybe dealbata, Clitocybe cerusata, and Omphalotus olearius). The first symptoms occur within 30 minutes to 2 hours. Depending on the mushroom species, they contain substances that determine the clinical picture of poisoning:
- muscarine;
- muscaridine.
With a predominance of muscarine content (in case of poisoning with mushrooms Inocybe Patujara, Amanita muscaria, Amanita panterina), the cholinergic syndrome prevails in the totality of manifestations:
- miosis;
- salivation;
- bronchorrhea;
- bronchoconstriction;
- paroxysmal sharp pain in the abdomen;
- nausea, vomiting, diarrhea.
Impurities of muscaridine and substances with similar effects are manifested:
- mydriasis;
- lacrimation;
- sweating.
Subsequently, signs of damage to the central nervous system appear: confusion, delirium, lethargy, disorientation, which later changes to a soporous state.
Type III poisoning involves phalotoxins and amanitotoxins, found, for example, in the death cap mushroom. Symptoms are distributed over a period of time:
- asymptomatic (up to 6 days);
- Gastrointestinal disturbances (occur suddenly, often not associated with the mushrooms, as several days have passed since their ingestion. Symptoms of gastroenteritis develop—diarrhea, vomiting, abdominal pain. Lasts three days. Fatalities during this period are rare);
- Phaloid hepatitis (lasts 2-3 weeks. Symptoms of acute renal failure and liver failure are observed: jaundice of the skin, hemorrhagic syndrome, abdominal pain, impaired consciousness, convulsions, coma, the occurrence of oligo-, anuria. During this time, fatal outcomes most often occur);
- exit (reduction in the intensity of symptoms).
Pickled mushroom poisoning
Poisoning from pickled mushrooms is possible. In this case, the clinical picture most often presents as botulism. After 4-5 hours, gastrointestinal symptoms, gastrointestinal paresis, and intoxication develop.
The clinical picture is quite pronounced. The patient experiences nausea, vomiting up to 10 times a day, and epigastric pain. Within 60 minutes, diarrhea gives way to constipation, a feeling of abdominal bloating, and increased gas production.
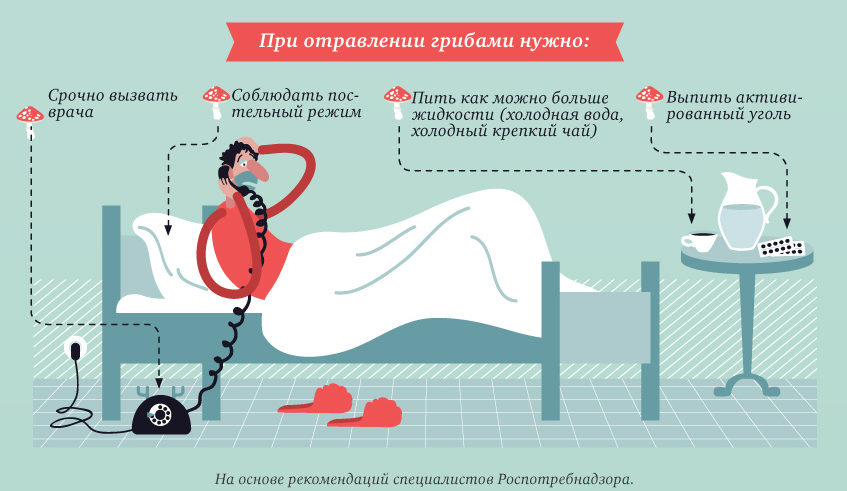
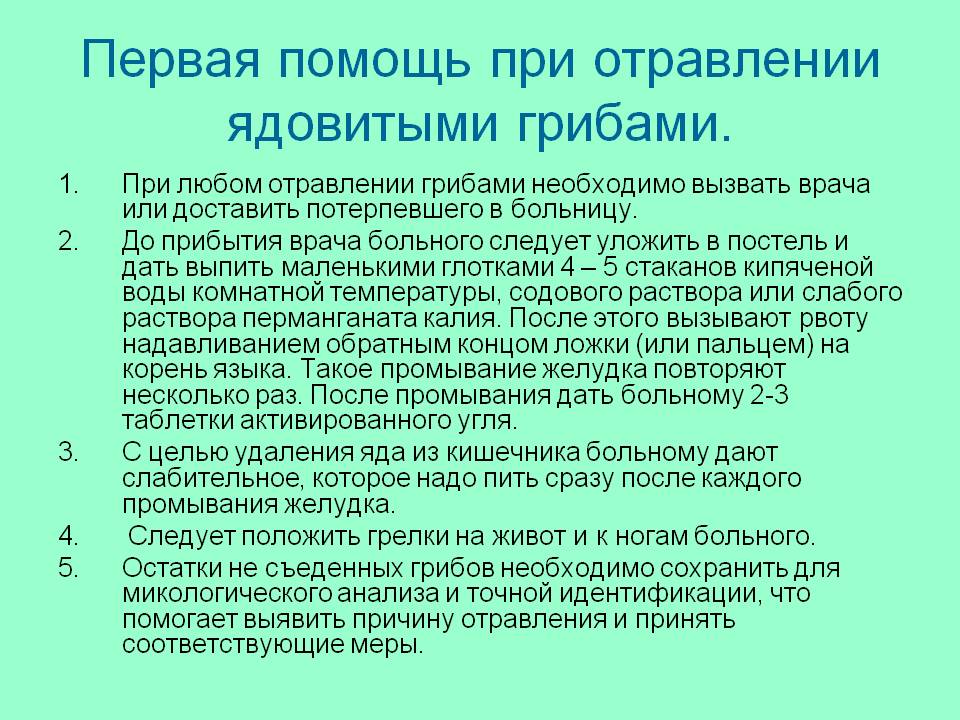
First aid at home
At the pre-hospital stage, at home, the following algorithm of first aid manipulations should be performed:
- Examination of the patient during vital function impairment. Depending on the type of impairment, airway patency is checked, and impaired ventilation and circulation are restored through mouth-to-mouth and mouth-to-nose resuscitation, as well as chest compressions.

Actions in case of mushroom poisoning - If consciousness is preserved and there are no hemodynamic disturbances, the stomach is lavaged with a thick tube or vomiting is induced (if the patient is conscious). Emetics (syrup of ipecac, etc.) are not indicated.
If disturbances in consciousness (stupor, coma) or hemodynamic parameters are detected, they are addressed through resuscitation measures. Gastric lavage is postponed until the patient is hospitalized in a specialized intensive care unit.
The ambulance team carries out the following activities:
- Activated charcoal mixed with laxatives (sorbitol) can be administered orally or through a stomach tube. Laxatives are not prescribed in cases of diarrhea.
- If symptoms of muscarine intoxication predominate, Atropine 0.1% is administered intravenously at a dose of 1-3 ml until clinical signs of moderate atropinization are obtained.

Procedure for providing first aid - If symptoms of muscaridine intoxication predominate, Physostigmine 0.5-2 mg or Galantamine 0.5-0.75 mg is prescribed intravenously as an antidote.
- Treatment for seizures, if they occur, differs little from the standard therapy for similar cases. GABA is administered intravenously at a dose of 100-150 mg/kg, or Sibazon (0.5 mg/kg), or Diphenin (15-20 mg/kg) is administered slowly, diluted in 50-100 ml of 0.9% NaCl solution.
- Next, hospitalization in a specialized intensive care unit is necessary.
Further treatment
At the hospital stage, the following set of measures is carried out, which necessarily takes into account everything that was done before the patient’s admission to the hospital:
- If vital functions are not restored, these disorders must be eliminated.
- In case of relapse of cholinergic syndrome: Atropine 0.1% at 0.001-0.003 mg/kg until moderate atropinization occurs.
- If anticholinergic syndrome develops, Physostigmine should be taken again as needed after 20-30 minutes, Galantamine 0.5-0.75 mg per day in 4 doses.

Anticholinergic syndrome - Anticonvulsants - in case of recurrence of seizures (in half doses).
- Infusion therapy: in patients with severe water-electrolyte losses - infusion solutions bolus 15-20 ml/kg of body weight (0.9% NaCl, Acesol, Disol, Trisol, Ringer's solutions, Ringer's lactate, Hartman), then therapy is carried out under the control of diuresis, central venous pressure, turgor and moisture of the skin, mucous membranes, filling of the subcutaneous veins, and lung auscultation data.
- In the absence of water-electrolyte losses, crystalloids, 3-4% sodium bicarbonate solutions, HEC preparations, Rheopolyglucin, Rheosorbilact, etc. (up to 40-50 ml per kg per day) are prescribed; if vomiting and diarrhea continue, the deficiency is replenished accordingly.
- If there is no stool colored by the activated carbon taken within 7-8 hours after the initial dose, re-prescribe half the dose of laxative.
- If vomiting and diarrhea continue, antiemetic and antidiarrheal drugs are not prescribed in order to improve the spontaneous cleansing of the stomach and intestines from fungal toxins.
- Symptomatic therapy.
https://www.youtube.com/watch?v=iB3555vNg28
Antidote therapy:
- Benzylpenicillin: 0.5-1 million units/kg/body weight per day intravenously during the first three days;
- Silibinin: 20 mg/kg per day orally (in the absence of vomiting) for 10-12 days. The daily dose is divided into 3 doses. The following medications contain silibinin: Silibor, Carsil, and Legalon.
Answers to frequently asked questions
In summary, it should be recognized that mushroom poisoning, particularly with amanita mushrooms, is often fatal. A positive outcome depends on prompt medical attention, which should be comprehensive and specialized, utilizing gastrointestinal decontamination methods, fluid resuscitation, extracorporeal detoxification, and early administration of antidotal agents.



















 What are the benefits and harms of oyster mushrooms for humans (+27 photos)?
What are the benefits and harms of oyster mushrooms for humans (+27 photos)? What to do if salted mushrooms become moldy (+11 photos)?
What to do if salted mushrooms become moldy (+11 photos)? What mushrooms are considered tubular and their description (+39 photos)
What mushrooms are considered tubular and their description (+39 photos) When and where can you start picking honey mushrooms in the Moscow region in 2021?
When and where can you start picking honey mushrooms in the Moscow region in 2021?